HOPia HOSPITAL offers a
FULL platform in CARDIAC SURGERY:
-
–Open-heart surgery under extracorporeal circulation (CP bypass),
-
–Hybrid surgery (placement of a mitral V-Clamp device)
-
–Interventional surgery / mini-invasive ( balloon valvuloplasty for pulmonic stenosis, ACDO for PDA closure…), placement of pacemakers…
HOPia is recognised competent in open heart surgery, in particular for mitral valve repair
Greensmith, T. and Cook, S. (2021), Extracorporeal therapies in veterinary medicine:
what is currently performed in the UK? In Practice, 43: 71-76
https://cavalierhealth.org/mitral_valve_disease.htm#Dr._Sabine_Bozon_–_Franc
Our foreign customers are most welcome!

A TEAM SKILLED IN OPEN-HEART SURGERY & MITRAL VALVE REPAIR
Doctors Sabine and Jean-Hugues Bozon belong to the very private circle of open-heart surgery teams. Thanks to their many years practising in this field, they have set up a 100% French team of professionals (surgeon, instrumentalists, cardiologist, perfusionists, anaesthetists, highly trained nurses…) able to perform open-heart surgery.
OTHER PROCEDURES under cardiopulmonary bypass
Apart from Degenerative Mitral Valve Disease, we operate on other canine and feline congenital heart diseases such as :
- Mitral dysplasia / stenosis
- Tricuspid dysplasia / stenosis
-
Pulmonic stenosis
- Atrial septal defect
- Ventricular septal defect
- Patent ductus arteriosus
- Cor triatriatum (sinister/dexter)
DEGENERATIVE MITRAL VALVE DISEASE (DMVD)
HOPia’S PATIENT CARE AND MANAGEMENT
Dog going for a walk 2 days after mitral valve surgery at HOPia

WHICH DOGS ARE AT RISK OF DEVELOPING DMVD?
DMVD is the most common acquired cardiac disease encountered in dogs. Small breed dogs over 5 to 7 years of age are particularly at risk. Cavaliers (for which a genetic predisposition has been identified), Dachshunds and Chihuahuas may have an early onset of the disease.
DMVD usually has a slow progression and all dogs may not develop clinical signs.
WHAT IS
DEGENERATIVE MITRAL VALVE DISEASE (DMVD)?
The heart has four valves (aortic, mitral, tricuspid, pulmonary), all of which can be concerned by the degenerative disease, although the mitral valve seems to be predominantly affected. The mitral valve is located between the left atrium and the left ventricle. The blood normally flows from the atrium to the ventricle, the latter will then contract strongly in order to eject the blood through the aorta to the rest of the body. The mitral valve, once closed, prevents the blood from returning to the atrium during ventricular contraction, allowing a unidirectional aortic flow. With DMVD, the mitral valve’s structure is modified into a thick and irregular flap which doesn’t close very well. As a consequence, it leaks, enabling the blood to reflux in the left atria during ventricular contraction.
Concurrent tricuspid degenerative disease is presented by 30% of these small breed dogs. More rarely, the aortic and pulmonary valves can be affected.
DMVD is a progressive process which worsens over time, especially in small breed dogs. The pressure within the left atrium gradually increases secondarily to the chronic leakage through the mitral valve. It can also present with an acute onset in case of a primary chordae tendineae (cords connecting the valve to the left ventricular myocardium) ruptures. An acute increase of the left atrial pressure will induce an accumulation of blood upstream from the left atrium, namely, the pulmonary veins and lungs, ultimately leading to pulmonary oedema (« water in the lungs »). When this occurs, it is said that the dog is in Congestive Heart Failure (CHF).

WHAT ARE THE CLINICAL SIGNS OF DMVD?
Pulmonary oedema is a major cause of dyspnea (difficulty to breathe) because the lungs are filled with fluid instead of air. The clinical signs associated with CHF are : lethargy, exercise intolerance, cough, increase in respiratory rate and amplitude of breathing movements. If one of those clinical signs is identified, a veterinarian must be contacted urgently.
IS THERE A MEDICAL TREATMENT?
Unfortunately, no medication exists to slow or stop the mitral valve degenerative disease.
In case of minor leakage with no heart remodelling, no medication is needed and the dog will have serial heart-scans to monitor the progression of the disease over time. When the leakage increases in volume and the left atrial starts dilating, a drug called « pimobendan » has proven to be very efficient in delaying the onset of CHF. This medication both reduces the cardiac workload by dilating the blood vessels downstream from the heart, and enhances its pumping action.
Once the dog has suffered from a CHF, other medications will be added to its treatment plan, the most important being diuretics like furosemide. Other drugs can be used, like benazepril, spironolactone, torasemide, sildenafil, entresto, etc.
Furosemide is a diuretic, which means that it promotes micturition therefore reducing fluid retention and delaying fluid build-up in the lungs.
HEART SURGERY
FOR MY DOG AT HOPia

DOES MY DOG NEED SURGICAL MITRAL VALVE REPAIR?
In order to determine the stage of heart disease your dog is suffering from, we will conduct an extensive set of medical pain free tests.
It includes:
-
chest radiographs (2 lateral views expi/inspi and 1 ventro-dorsal view)
-
cardiac ultrasound with colour Doppler (images & videos are needed for the assessment)
-
electrocardiogram
-
NT-proBNP dosage
Picture on the left : Dr JH Bozon leading the cardiac surgery
THE ACVIM CLASSIFICATION
Staging a dog’s heart disease is important to follow the recommended therapeutic guidelines established by the 2019 ACVIM (American College of Veterinary Internal Medicine) consensus to best treat the condition. The therapeutic plan will also be adapted individually thanks to the complete description of the disease provided by the analysis of each dog.
ACVIM STAGE A
This class comprises all animals « at risk » (because of their pedigree or breed) of developing the disease but that do not have any heart abnormalities upon clinical examination. They do not need any treatment.
For instance, a new-born Cavalier King Charles Spaniel is in Stage A because this breed is predisposed to DMVD even at a young age.
ACVIM STAGE B
This class comprises dogs with a heart murmur without any other clinical signs. This stage is further subdivided into Stage B1 and B2.
-
The sub-stage B1 includes dogs without radiographic or echocardiographic evidence of cardiac remodelling in response to DMVD (no evidence of left atrial or ventricular enlargement) ; these dogs don’t need any treatment
-
The sub-stage B2 includes dogs with radiographic and/or echocardiographic evidence of left-sided heart enlargement ; these dogs will benefit from the use of pimobendane (proven by the EPIC study – 2016)
SURGERY MIGHT BE RECOMMENDED in case of a very ADVANCED B2 stage
ACVIM STAGE C
This class comprises dogs showing, or that have showed, clinical signs of CHF (i.e. that have suffered from respiratory failure because of chronic or acute pulmonary oedema). At this stage, at least a bi-therapy must be instituted (pimobendane + furosemide +/- spironolactone +/- benazepril). Some dogs will also need sildenafil in case of superimposed pulmonary hypertension.
Life expectancy at this stage is limited and statistically reduced to 6-18 months after the first onset of pulmonary oedema.
SURGERY IS OFTEN RECOMMENDED but it is a case-by-case assessment
ACVIM STAGE D
This class comprises dogs unresponsive to medical treatment, in other words, dogs receiving upper-range dosage of diuretics and still presenting clinical signs of CHF. At this stage, the cardiologist might prescribe more drugs like amlodipine, cough-suppressants, anti-arrhythmics, other diuretics (torasemide, thiazides),beta blockers (carvedilol), sildenafil, etc. Hospitalisation for oxygen therapy and IV administration of the drugs is often necessary at this stage.
SURGERY MIGHT BE RECOMMENDED (sometimes the only option) BUT THE SUCCESS RATE IS MUCH LOWER
At HOPia, we mainly operate on dogs suffering from EARLY stage C OR LATE STAGE B2.
We DO NOT operate stage D cases.
In order to ensure a reasonable success rate, the maximum tolerate age to consider surgery is 10 years old. Sometimes we accept dogs between 10 and 12 yo. The success rate drops down after 12 years of age and we do not advise the surgery because of the uncertain peri-operative outcome.

SURGICAL VS MEDICAL TREATMENT?
Firstly, we require a complete cardiac work-up in order to evaluate if surgery is among the therapeutic options. We then evaluate the risks of heart surgery versus those of medical treatment. Surgery is never elected if the dog has not been on heart medication for at least 3 months.
Surgery for mitral valve repair might be indicated in case of:
-
severe mitral valve prolapse
-
grade 4 mitral regurgitation (extending into the pulmonary veins)
-
severe primary chordae tendineae rupture
-
significant dilation of the left atrium
- severe irreversible mitral annulus dilation
If surgery is an option, we require medical tests to insure that the dog is not suffering from other diseases that could compromise surgery or the post-operative outcome.
In any case, our goal is to make sure that your pet gets the best treatment recommendations considering his global health status.
PAPERWORK
TO GET YOUR DOG OPEN HEART SURGERY
Cardiac surgery planning is a 2-month process (except emergency) – here are the 10-key steps in chronological order
01
Candidacy evaluation (cardiac status)
Please send us, through the contact formulary OR at contact@hopia.fr, your dog’s latest heart-scan (pictures + video loops) and chest radiographs, his relevant medical history and his ongoing treatment plan.
-
Detailed recent physical examination and relevant history
- Current medication with names and dosages
-
Latest detailed cardiac ultrasound scan (images and more important the video loops including colour)
-
Latest chest radiographs
- Electrocardiogram (ECG)
-
Arterial blood pressure measurement
- NT-ProBNP dosage

02
Ask your veterinarian to perform the following tests (please send the complete digital version of these tests) 2 months prior to the presumed date of surgery
-
NT-ProBNP and Cardiac Troponin I dosages
-
Full abdominal ultrasound scan (must be particularly closely examined : adrenal glands for features of Cushing’s disease, pancreas for signs of pancreatitis, search an occult tumour present)
-
Blood tests : haematology, complete biochemistry panel, electrolytes, C-Reactive Protein, SDMA, cPLi, T4, TSH, 4DX
-
Urinary Bacterial culture (sampling by cystocentesis)
-
Full coagulation profile including antithrombin III dosage, D-dimer and fibrinogen
-
Blood type (DEA 1.1)
03
Interpretation of the results, validation that your dog fits the criteria for open heart surgery
04
Date scheduling for your dog’s surgery / a financial deposit is required to secure the surgical slot blocked off.
05
Possible refinement of the therapeutic plan in order to optimise preoperative conditions
06
Additional exams potentially necessary before surgery – we need an updated cardiac ultrasound recheck 2 weeks before the surgery date
07
Plan to arrive between 1 to 5 days prior to surgery at HOPia (determined case by case)
08
Pre-operative check-up at HOPia the day before surgery
09
SURGERY DAY
10
7 to 10 days hospitalisation in the Intensive care Unit
General guidelines
of open heart surgery for DMVD
Open-heart surgery implicates a large number of veterinarians working together, and the use of many machines and consumables.
The procedure’s success relies on the training, professionalism and cohesion of this team, from the first second to the last of this 7 to 10-day process.
MACHINES AND CONSUMABLES
Apart from the extracorporeal circulation machine, key pieces to the procedure, the necessary equipment is as follows:
-
2 anaesthetic machines (isoflurane or sevoflurane)
- 1 ventilator
-
1 complete multiparameter monitoring device (ECG, heart rate, respiratory rate, invasive arterial pressure, central venous pressure, non-invasive arterial pressure, pulse oximetry, capnography, FiO2, fraction of anaesthetic gas expired, oesophageal and rectal temperatures)
-
1 thermic generator able to warm up and cool down the body to the adequate temperature according to the step of the procedure
- 1 four-plane tilting surgical table
-
1 ultrasonographic scanner with colour Doppler and paediatric trans-oesophageal probe
-
4 syringe and 2 perfusion pumps
-
1 real-time clotting-time measurement machine
-
1 real-time blood gas analyser
-
1 real-time haematology and biochemistry analyser
-
1 real-time electrolytes analyser
-
1 implantable defibrillator equipped with paediatric pads
-
1 pace-maker
-
fresh whole blood from a donor previously tested as compatible with the operated dog
-
blood typing tests
-
cross match tests to perform between donors and receivers
-
cell-saver (a machine enabling auto-transfusion)
-
a cardioplegic solution (that stops and protects the heart during the valve repair)
-
frozen sterile saline
-
ice
-
numerous consumables and injectable drugs
-
traditional equipment : aspiration, cautery with delicate calibration (thermofusion), microsurgery equipment, customised equipment (catheters, tubing..)
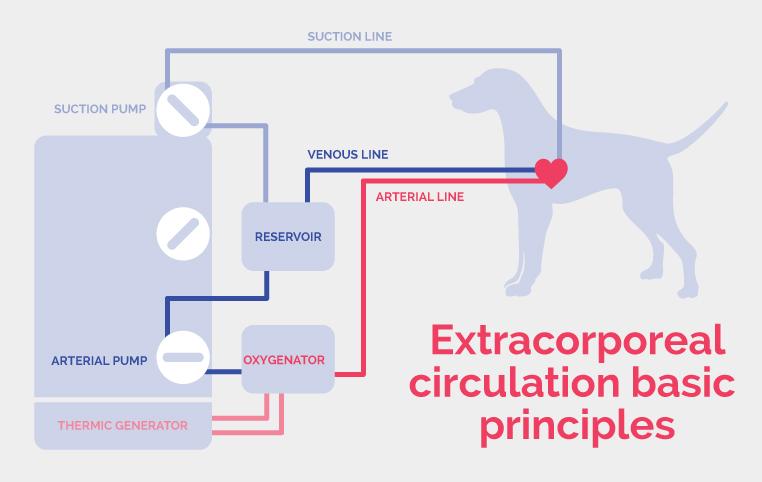
Heart-lung bypass machine – centerpiece of the intervention
The technical and human platform are important, the team must have a perfect cohesion but the most crucial point is the heart-lung bypass machinery which represents quite a challenge in small individuals.
At HOPia, we are able to operate on Chihuahuas as small as 1,4 kg.
In small breed dogs, extracorporeal circulation is a technical challenge because of their very small total blood volume. The tubing is customized to small individuals such as miniature dogs and cats. Heart-lung bypass procedures induce cardiac arrest, thus enabling the surgeon to repair the valves on a motion-free heart. The bypass takes over the lung and heart (pump) functions during the intra-cardiac surgical time.
What are the diffrent parts of the heart-lung bypass machine?
-
a venous line
-
two suction lines, one for the thoracic cavity and the other for the heart cavity
-
a tank
-
an oxygenator
-
a thermic generator able to control the blood and thus the body temperature
-
two suction pumps
-
an arterial line
-
an intermediate line for arterial blood sampling
-
a monitor displaying all the parameters’ live values
-
an anaesthesia circuit for isoflurane and sevoflurane
- an hemofilter
- a monitor displaying all the parameters’ blood values
The perfusionist, working hand-in-hand with the surgeon and the anaesthetist, must master the extracorporeal circulation technique for the procedure to be a success.
Doctors Sabine and Jean-Hugues Bozon are the ones giving instructions to the perfusionist.
THE DIFFERENT STEPS OF THE PROCEDURE
It is important to maximise the number of steps that may be done on the conscious animal in order to reduce the anaesthetic time:
-
venous catheter placement in the two fore limbs
-
central venous line placement
-
arterial catheter placement in the hind limb
-
urinary Foley catheter placement
-
left thorax and neck clipping
The operating theatre is also prepared during that time.

The next steps are the following:
01. Premedication
02. General anaesthesia induction and intubation
03. Jugular vein and carotid dissection
04. Chest opening, lung reflection, pericardectomy enabling the access to the heart
05. Aortic and pulmonary artery dissection + aortic catheter placement
06. Induction of a state of hypocoagulability with monitoring of the clotting time
07. Cannulation of the jugular vein and carotid artery
08. Induction of partial then total extracorporeal circulation (cardiopulmonary bypass) with the heart-lung machine
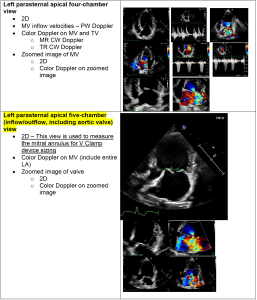
09. Transoesophageal hear-scan: a transoesophageal paediatric probe connected to an ultrasonographic scan equipped with colour Doppler is delicately inserted in the oesophagus in order to obtain successive images of the heart in median transversal and longitudinal cross-sectional planes. The surgeon analyses the mitral valve movements, the different segments and the regurgitation.
10. Body temperature cooling: the body temperature is progressively lowered to 28°C and maintained at that level thanks to a thermic generator integrated to the extracorporeal circuit
11. Cardioplegic solution injection in the coronary arteries to induce cardiac arrest
12. Heart opening and introduction of the suction lines
13. Pre-placement of the artificial mitral valve chordae tendineae to insure a proper repair of the ruptured chordae. Three to Five artificial chordaes are placed depending on the case.
14. Mitral annuloplasty: the aim is to tighten the mitral annulus in order to reduce the mitral regurgitation and thus to maintain a good systolic coaptation. The same material as the chordae is used (ePTFE). The mitral annulus is tightened based on the surgeon’s experience and the preoperative measurements.
15. The artificial mitral valve chordae tendineae are secured. The main challenge at this point is to find the perfect length and tension allowing optimal coaptation during closure of the mitral valve.
16. Left atrium suture and intracavitary gas removal under ultrasonographic monitoring (using the transoesophageal probe) and aortic de-clamping.
17. The heart is then restarted. The heart beat is expected to restart after the intracoronary recurrent cardioplegic injections are discontinued. Intra-thoracic heart massage is performed and sometimes a pacemaker is temporary set in place or ventricular defibrillation is needed.
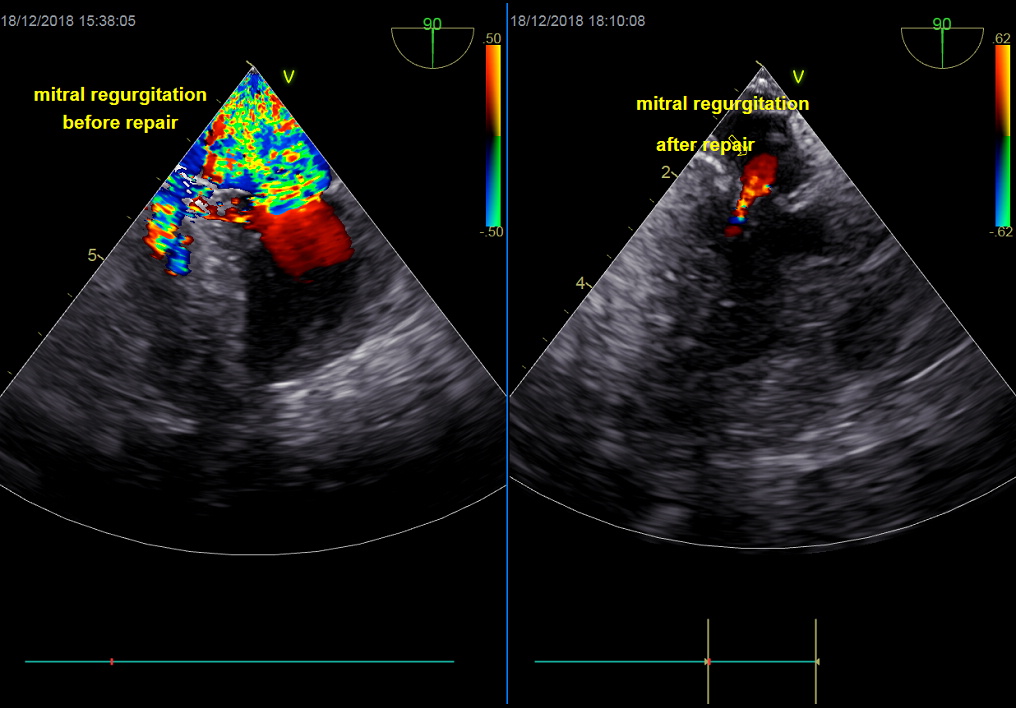
18. Control transoesophageal heart-scan: the mitral valve coaptation, residual mitral regurgitation, systolic function, ventricle blood volume and presence of gas are checked.
19. Body temperature is gradually increased and arterial pump flow is progressively reduced.
20. The carotid artery and jugular vein cannulas are withdrawn and the extracorporeal circulation is terminated.
21. Protamine, a heparin antidote is infused. Protamine can indeed induce severe hypotension, bronchospasm and increase pulmonary vascular resistance.
22. Chest closure (the pericardium is not sutured).
23. Thoracic drain placement
24. Very slow awakening over 2-3 hours. During this crucial phase, all of the vital parameters (ECG, invasive BP, CVP, HR, RR, SpO2, pCO2, temperatures) and ventilation are closely monitored and their return to a normal level is very progressively obtained. The clotting times are checked and must return to a normal level. The dog is then transferred to the intensive care unit where an oxygenated and temperature and humidity controlled cage awaits (ICU Menix Operation System cages).
Once the mitral valve is repaired and the new chordae are set in place, the mitral prolapse is diminished if not abolished, the valve coaptation is appropriate and the mitral regurgitation is markedly reduced. The left atrium has an amazing plasticity which allows it to reduce to a normal size in sometimes no more than a week post-operatively if the tissue is still healthy enough and if surgery hasn’t been performed to late.
During the post-operative hospitalisation period, the treatment plan for congestive heart failure is adjusted and then often discontinued. Several platelet inhibitors and blood thinning drugs are prescribed to prevent thrombosis, the most common complication observed during that phase.
The post-operative care is a real challenge!
It is a very critical phase during which the dog may die because many organs have suffered from the extracorporeal circulation, even the blood, to start with, because it has flown outside of its usual body. A complete blood panel, urinalysis, radiographic and ultrasonographic scans are performed daily during the week following surgery. 24/24 monitoring is done by a dedicated personal « cardiac surgery trained » nurse.
Apart from thrombosis (clot formation), the possible complications are:
-
Sudden cardiac arrest
-
Respiratory failure
-
Haemorrhage
-
Anaemia (sometimes haemolytic)
-
Acute pancreatitis
-
Arrythmias
-
Diaphragmatic paralysis
-
Coronary or cerebral gas embolism
- Systemic inflammatory response syndrome
-
Acute right sided-heart failure
-
Acute pulmonary arterial hypertension
-
Focal infection among which the worse is endocarditis
-
Stroke (hypoxic, haemorrhagic or thrombotic)
- …
Open-heart surgery is a highly risky procedure : All the signs of possible complication development are checked during the week following surgery and the treatment plan is adjusted accordingly to avoid a fatal outcome.
HEART-SURGERY
WHAT RESULTS TO EXPECT?
If the surgery is a success, your pet will always have a healed heart as long as you respect the post-surgery exercise restrictions.
About 80% of the dogs will stop medication after 3 months. A diminution of the heart cavities will be observed, a significant loss of mitral regurgitation that will become moderate or inexistent, enabling your dog to live normally without having breathing difficulties or being tired.
Pictures on the right: Mitral valve repair performed by Dr JH Bozon. Top : Peroperative Transoesophageal Echocardiographye (Dr Sabine Bozon). Bottom : Post-operative trans-thoracic Echocardiography (Dr Sabine Bozon)
The post-operative risks
Death on the operating table can occur; it is usually due to hemorrhage or low blood pressure or acute pulmonary hypertension…. The worse the cardiac failure stage, the riskier. There is also a high risk of death during the post-operative week in intensive care, when many complications may occur.
Apart from thrombosis (clot formation), the possible complications are:
-
Sudden cardiac arrest
-
Respiratory failure
-
Haemorrhage
-
Anaemia (sometimes haemolytic)
-
Acute pancreatitis
-
Tachycardia
-
Diaphragmatic paralysis
-
Coronary or cerebral gas embolism
- …
- Systemic inflammatory response syndrome
-
Acute right sided-heart failure
-
Acute pulmonary arterial hypertension
-
Focal infection among which the worse is endocarditis
-
Stroke (hypoxic, haemorrhagic or thrombotic)
- Myocardial infarct
- …
We are equipped to detect and treat most of these risks. A complete health check is performed on a daily basis along with many other analysis or diagnostic imaging. In a few of cases, an incurable complication occurs.

Open-heart
cardiac surgery schedule
Open-heart surgery
Regular cardiac surgeries are performed throughout the year at the HOPIA clinic except if the whole team can’t be present (vacation, sickness…).
.
Open heart surgery requires the presence of at least 10 professionals who are trained in this very complicated procedure.
The surgeries are organized about 2 months in advance (except emergency).
Given the many requests from all over the world, our schedule is usually very full but we give priority to emergencies.
Non-urgent surgeries are likely to be postponed in order to help a dog who is suffering.